Let me tell you a story most people don’t expect. In a bustling Melbourne conference, leaders share more than stats—they bring life to the invisible challenges Deaf communities face. Their stories aren’t just numbers—they're about that dinner table where only one sibling is Deaf, or a parent awkwardly gestures rather than signs because they never learned Auslan. I’ve seen firsthand how a single caring interpreter—or an overlooked caption—can change an entire medical journey. This model is about giving those stories the space and solutions they deserve. Let’s unpack what Victoria’s Deaf and hard of hearing mental health model is really about—by the people, for the people, with honesty and a few real-life surprises.
Service Design Overview: Building for Real Lives, Not Just Checklists
When you think about Deaf mental health services in Victoria, it’s easy to imagine a system built from the top down—policies written in offices, checklists ticked off, and decisions made without real input from the people who use those services. But the new approach in Victoria is different. Here, the design of mental health and wellbeing services for the Deaf and hard of hearing community is shaped by the community itself, not just by experts or government officials.
Community-Led Organisations at the Heart
This model was created through a direct partnership between Deaf Victoria—the state’s leading advocacy body—and Deakin University, whose research has set international standards for deaf community support. Instead of imposing solutions, the process focused on listening. As Dr. Amy O’Shea put it,
“It came from a deep interconnectedness and trust that had been given and placed in me by people over time...”This trust is what makes the model unique. You can see it in every step, from the first conversations to the final plans.
Major Investment for Real Change
The Victorian Government has backed this approach with serious funding: $4.2 million allocated from 2023 to 2025 for diverse community mental health projects. Out of this, $230,000 was awarded directly to Deaf Victoria for designing a care model and delivering deaf cultural competency training for mental health workers. This isn’t just about money—it’s about recognising the importance of community-led organisations and giving them the resources to lead.
Design With, Not For: Core Values in Action
At the core of this service design are values like inclusion, cultural safety, and continuous improvement. The idea is to design with the Deaf community, not just for them. This means every policy, every training session, and every service is shaped by people who truly understand the mental health challenges deaf and hard of hearing individuals face.
Research-Driven, Needs-Led
Research shows that community-driven data is essential. In 2023, the Deaf Australia census gathered responses from over 850 Deaf and hard of hearing adults. These findings guide every detail of the new model. For example, about half of the respondents reported a formal mental health diagnosis, while the other half identified with informal or self-recognised mental health issues. This highlights how barriers are often rooted in communication and culture—not just clinical factors.
- Direct partnership with Deaf Victoria and Deakin University ensures authentic representation.
- Government investment of $4.2 million (2023-25) supports innovation and workforce training.
- Core values: Inclusion, cultural safety, and continuous improvement.
- 850+ census responses drive policy and service design.
- Lived experience is central—barriers are often about communication, not just diagnosis.
By focusing on community-led organisations and research, Victoria is setting a new standard for mental health and wellbeing services. This approach, supported by Deakin University deaf community research and significant Deaf Victoria mental health funding, is designed to meet real needs—not just tick boxes.

Community Engagement: Nothing About Us Without Us
When it comes to mental health and wellbeing for the Deaf and hard of hearing community in Victoria, true progress starts with community-led organisations. You see this in action at every stage—from the first idea to the final rollout. Deaf community leaders, clinicians, and academics work together, sharing real power and responsibility. This isn’t just a token gesture. It’s a model built on trust, respect, and lived experience.
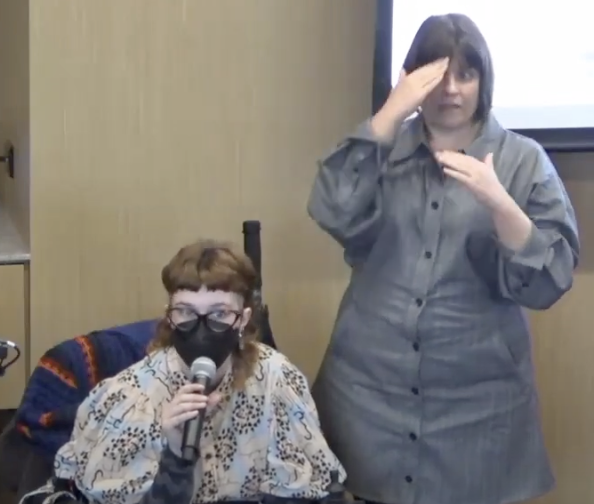
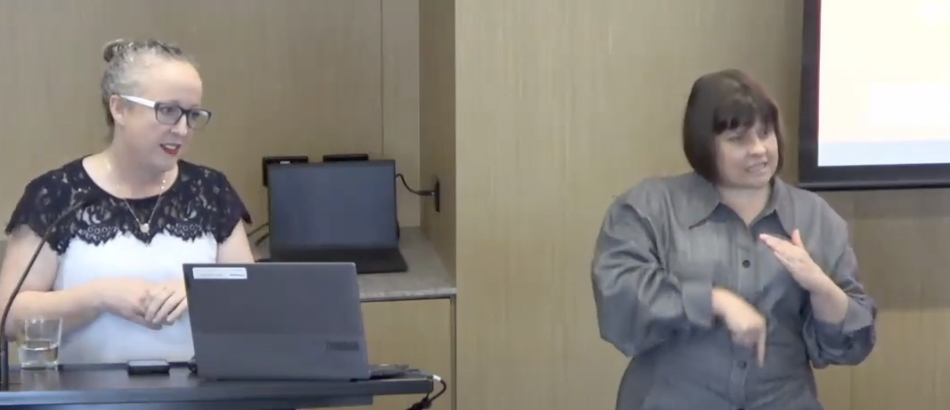
At events like those led by Deaf Victoria and Deakin University, you’ll notice something different right away. The first words are not about the project itself, but about recognition. There are formal acknowledgements to the Wurundjeri people of the Kulin Nation, and to Aboriginal and Torres Strait Islander communities. This is followed by heartfelt tributes to Deaf and hard of hearing individuals with lived experience of mental health challenges—those who have faced trauma, neurodiversity, substance use, or addiction, as well as their families, carers, and supporters.
This culture of recognition extends to those who have paved the way. Leaders and advocates from the Deaf community, both past and present, are named and thanked. Their tireless advocacy and courage are seen as the foundation for today’s progress. Even those who are no longer with us are remembered, their initials and names displayed with respect. This is not just ceremony—it’s a reminder that community-led organisations are essential for culturally safe care. Research shows that long-term trust and reciprocity are what make these projects work.
Diversity is always at the centre. Presenters openly acknowledge the complex realities faced by Deaf and hard of hearing people. They talk about trauma, neurodiversity, intersecting cultures, and the unique challenges of substance use. This openness makes the research more personal and relevant. It’s not about outside experts coming in with ready-made answers. Instead, it’s about learning from decades of lived experience. As Dr. Amy O’Shea from Deakin University puts it:
"Again and again, the Deaf community have given me the opportunity to learn from them. I've taken on their wisdom and their experiences, and I'm incredibly privileged to be in that position."
This approach is echoed in the ongoing partnership between Deaf Victoria and Deakin University, which dates back to 2015. Their collaboration is a model for how community-led organisations and academic research can work hand-in-hand. It’s not just about research for its own sake. It’s about making sure that every step is informed by those with real, lived experience.
You’ll also see that allies are named and thanked. This reflects a “community-as-expert” approach, rather than assuming that expertise only comes from outside. Presenters often share how their own journeys—sometimes spanning 25 years or more—have been shaped by the Deaf community’s generosity and wisdom. This continuous learning and feedback loop means that the model itself keeps evolving, always shaped by real-world needs and insights.
In Victoria, empowering Deaf and hard of hearing mental health is not an afterthought. It’s a process led by those who know it best, supported by research, and grounded in respect for diversity and history. If you want to understand what real community engagement looks like, this is where you start.
Accessibility Measures: Breaking Barriers One Step at a Time
When you think about mental health support for Deaf and hard of hearing people, accessibility isn’t just a buzzword—it’s the foundation. In Victoria, there’s a growing recognition that true accessibility means more than ramps or hearing loops. It’s about making sure Auslan interpreter access in mental health settings is standard, not a rare accommodation. Live remote captions, visual information at events, and Auslan translators are now expected as part of therapy and family services, not optional extras.
But why is this so important? Let’s look at the numbers. Research shows that about 97% of Deaf children are born to hearing parents. Here’s the kicker: only about 8% of those parents learn Auslan, the sign language used in Australia. That means most Deaf children grow up in homes where their primary language isn’t spoken or signed. The gap starts early, and it’s not just about language—it’s about connection, culture, and emotional wellbeing.
“So ninety five to ninety seven percent in Australia of hearing parents, have deaf children. So the deaf children that are born, ninety seven percent of those deaf children have hearing parents.” – (Rammus McQuay)
This cultural and communication gap can quickly become a mental health barrier. Studies indicate that 50% of Deaf participants had no formal diagnosis—often because they couldn’t access assessments or communicate their needs clearly. For many, self-diagnosis or confiding in trusted friends is the only path to support. Imagine trying to navigate therapy support assessments when the system isn’t designed for your language or culture.
Barriers aren’t just technical or physical. They’re woven into family life, school experiences, and even the way care is delivered. Misunderstandings, teasing, or exclusion can all trip up care and connection. That’s why Victoria is focusing on cultural competency training for mental health professionals. It’s not enough to know the basics of mental health—you need to understand Deaf culture, the importance of Auslan, and how to work with interpreters. This training is now a core part of the workforce development strategy, as research and government initiatives highlight the need for culturally safe and responsive services.
You’ll notice these changes in real ways. Public events now feature Auslan interpreter and captioning services as a matter of course. Therapy and family services are being redesigned to include visual information and clear communication at every step. Early intervention programs, like those offered by Deaf Connect, focus on family support, communication, and education—helping to shape better mental health outcomes from the start.
Victoria’s approach is about more than ticking boxes. It’s about recognizing where misunderstanding, teasing, or exclusion can derail care, and actively working to fix it. By addressing access challenges—whether it’s sign language exposure, family dynamics, or bullying—the system is slowly becoming more inclusive. The hope is that, with these measures, Deaf children and adults will find it easier to access the mental health care they deserve, without having to fight for every step.
Practical Benefits: What It Means in Everyday Life
When you think about mental health and wellbeing for the Deaf and hard of hearing community in Victoria, it’s easy to focus on big-picture changes. But what does it actually look like, day to day? The new approach to therapy and family services is designed to make a real difference in your life, not just in theory but in practice.
Understanding the Real Stresses—And Responding with Support
If you’re Deaf or hard of hearing, you may know what it’s like to navigate two worlds. There’s the internal stress: growing up, you might feel lost, wondering where you fit. Are you Deaf, or are you hearing? Do you belong at the “quiet” dinner table, or the lively one where sign language flies? This identity confusion is real, and it’s something many people experience. Then there are the external pressures—being left out of conversations, feeling like you’re missing out, or even being teased or bullied at school or work.
That’s why Victoria’s support services for deaf mental health are now built around your lived experience. Mental health workers are trained with the community, not just for it. They understand the unique challenges you face, and they’re ready to listen—whether your needs are “officially” diagnosed or simply self-identified.
Early Intervention Therapy Support: Building a Healthier Future
Research shows that early intervention therapy support is key. When Deaf children and their families get extra support early on, it lays the foundation for better mental health and wellbeing as they grow. As Deaf Connect puts it:
"Early intervention programs for deaf children emphasize family support, communication, education, and technology needs to improve mental health outcomes."
That means more than just therapy. It’s about family therapy, speech-language support, and programs that involve everyone—parents, siblings, and carers—so no one feels left out or misunderstood.
Allied Health Teams: Working Together, Not Alone
Gone are the days of “lone wolf” therapists. Now, allied health teams—including interpreters, family therapists, and peer mentors—work together. This multidisciplinary approach means you get a team that advocates for you, not just a single professional. Peer-led mentorship and community workshops are part of the picture, too, so you can connect with others who truly “get it.”
Listening to Every Voice—Even If It’s Not Diagnosed
One of the most important changes is that people who self-identify their mental health needs are finally being heard. You don’t need a clinical diagnosis to access therapy support assessments or to join a support group. If you feel you need help, there’s a place for you.
- Peer and family support is now offered in all new programs.
- Therapy services include early intervention, allied health, and speech-language support.
- Ongoing feedback from Deaf clients and carers shapes the services you receive.
The result? Not just crisis support, but better everyday care—peer mentoring, multidisciplinary care, and proactive outreach that make every step more accessible and supportive for the Deaf and hard of hearing community.

Future Directions: Beyond Models—Toward Empowerment and Equity
When you look at the future of mental health reform in Victoria, especially for the Deaf and hard of hearing community, it’s clear that we’re moving beyond just building new models. The focus is shifting toward real empowerment and lasting equity. If you’ve followed the journey so far, you’ll know that mental health workforce development is not just about training—it’s about transformation. Victoria’s commitment to ongoing Deaf cultural competency and the regular hosting of mental health interpreting summits is setting a new standard for what professional development can look like.
The upcoming 2025 Summit for Mental Health Interpreting is a perfect example. This summit isn’t just a one-off event; it’s part of a continuous cycle of research, feedback, and improvement. Professionals from across the sector will gather to deepen their understanding, share lived experiences, and refine their skills. As research shows, these feedback loops are essential—they underpin long-term equity and real impact. The summit will also offer advanced pathways for interpreters and mental health professionals, ensuring that access to mental health services continues to improve for Deaf, DeafBlind, and hard of hearing individuals.
But there’s something even more important happening here: a shift in mindset. “Reciprocity” is becoming more than just a buzzword. There’s a real hope—backed by the work of organisations like Deaf Victoria, Deakin University, and Deaf Connect—that mainstream mental health care will not only listen to Deaf wisdom, but actively learn from it. This is about moving from a place where feedback is merely tolerated, to a place where it’s truly valued and integrated. As Dr. Amy O’Shea put it:
"I'd like to ask you all to think about how you too can make the learning that you get today, the learning that you've had from deaf people in the deaf community over time...so that we can together improve health and well-being for the Deaf community."
This invitation is for everyone—including you. How can you take what you’ve learned about Deaf community research, mental health services access, and cultural competency back to your own circles? How can you make it mutual, so that learning flows both ways? The answer isn’t always simple. Sometimes it means asking more questions than you answer. Sometimes it means sitting with discomfort, or letting go of old assumptions. But it always means staying engaged.
Sustained improvements in mental health services depend on ongoing workforce training, cyclical community engagement, and research that never stops asking, “What’s next?” The Victorian Government’s investment in mental health reform, along with the dedication of community-led organisations, shows that this work is just beginning. The Deaf mental health model is evolving—and what you do next, how you choose to participate, truly matters. The journey toward empowerment and equity is ongoing. Let’s keep moving forward, together.
TL;DR: Victoria’s Deaf and hard of hearing mental health model puts lived experience front and centre: community leadership, accessible tools, and better-trained care teams are making mental health services more responsive and empowering for all. It’s a leap toward wellbeing—together.
Congratulations on prioritizing mental health equity and designing services that are inclusive for the Deaf community. The content is truly enlightening. Take a look here: https://www.youtube.com/watch?v=yIRLemxvuR8.



